Inside the Arthritic Joint: How Focused Shockwaves Affect Synovium and Synovial Fluid
Focused extracorporeal shockwave therapy (ESWT) is a non-invasive treatment used in veterinary medicine for the treatment of osteoarthritis (OA). By delivering pressure waves to affected joints, ESWT can reduce pain and stimulate healing in tissues. This blog dives into how shockwave therapy impacts the joint’s synovial tissue, improving joint health and function in animals with OA.
Physiological Changes in Osteoarthritis? Synovial Tissue Under Attack
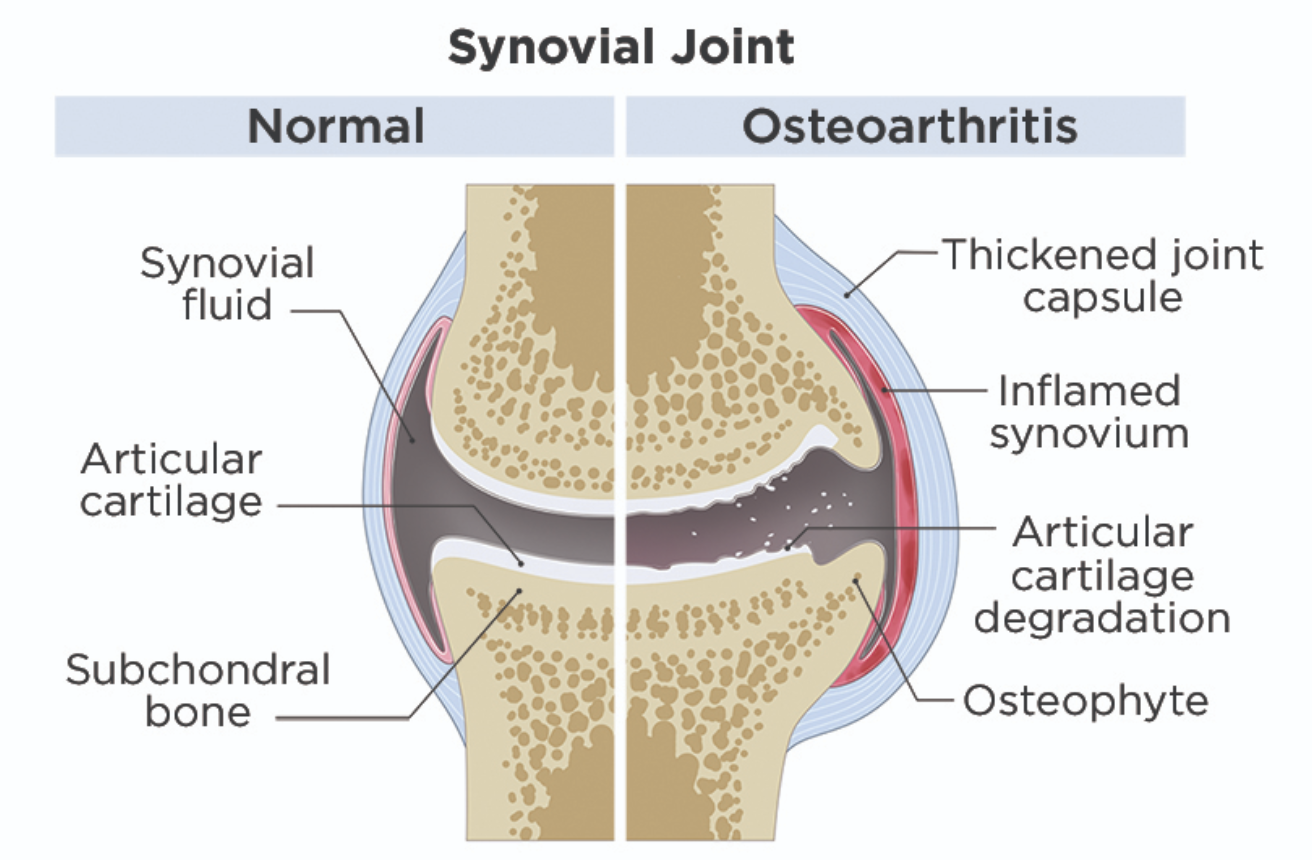
Osteoarthritis doesn’t only affect cartilage – it also disrupts the synovium and synovial fluid. A hallmark of OA is synovitis, or inflammation of the synovial membrane, in which the synovial lining becomes thickened and inflamed. The synovium is infiltrated by immune cells (macrophages, lymphocytes), turning it into an active source of inflammatory mediators 1. Chronic synovial inflammation produces pain (via nociceptive substances) and releases cytokines that further damage cartilage, creating a vicious cycle in the joint 1.
The synovial fluid also undergoes notable degradative changes in OA. Both the concentration and molecular weight of hyaluronic acid drop, and levels of lubricin are reduced, according to analyses of arthritic joints2. This causes the fluid to become less viscous and less effective at cushioning and lubricating the joint, especially as the joint often develops an effusion (excess fluid) that further thins it. At the same time, the fluid becomes a soup of inflammatory and destructive factors. Pro-inflammatory cytokines like interleukin-1β (IL-1β), tumor necrosis factor-α (TNF-α), IL-6, and IL-8 are found at elevated levels in OA synovial fluid1. These cytokines stimulate the synovium and chondrocytes to produce matrix-degrading enzymes and aggrecanases which actively break down cartilage collagen and proteoglycans. As a result, fragments of cartilage and bone end up suspended in the synovial fluid as debris from ongoing tissue damage. Overall, the synovial fluid in OA becomes more inflammatory and less protective: it loses its normal viscosity and nourishing quality and instead contains mediators that perpetuate pain and cartilage destruction.

How Focused ESWT Helps the Osteoarthritic Joint
Focused shockwave therapy can reduce synovial inflammation (synovitis). Shockwave therapy can significantly suppress the production of key pro-inflammatory cytokines within osteoarthritic joints. In animal models of knee OA, ESWT led to lower TNF-α levels in the synovial cavity, and in clinical studies on osteoarthritic knees, a single shockwave treatment caused a significant decrease in synovial fluid IL-1β and TNF-α concentrations (cytokines largely responsible for driving joint inflammation and cartilage breakdown)3. ESWT lowers the inflammatory signaling that keeps the synovial membrane in an irritated, overactive state.
Shockwave therapy interferes with the “pain-inflammation” cycle in arthritic joints. Substance P and CGRP are two neuron-derived peptides that promote pain perception and neurogenic inflammation in the synovium. Focused ESWT reduces levels of substance P in treated joints4. By depleting substance P (and likely dampening CGRP as well), ESWT helps break the cycle of pain and inflammation – leading to less vasodilation, reduced inflammatory cell recruitment in the synovium, and improved comfort for the animal.
Shockwave therapy also reduces oxidative stress in the joint environment. Osteoarthritic synovium produces high levels of nitric oxide (NO) and reactive oxygen species, which can damage tissues and induce chondrocyte apoptosis. Focused ESWT lowers NO levels in the synovial fluid of OA joints 5. Concurrently, it can boost antioxidant defenses; one study noted that synovial fluid superoxide dismutase (SOD, an antioxidant enzyme) activity increased after ESWT, indicating reduced oxidative stress in the joint 3. Less NO and oxidative damage provide a better environment for chondrocytes and synoviocytes. These anti-inflammatory and anti-oxidative effects lead to histologic improvements in the synovium: in a rat OA model, shockwave-treated joints showed a thinner synovial lining with far fewer inflammatory cells. ESWT can reverse synovial hyperplasia and inflammatory cell infiltration, restoring the synovial membrane closer to its healthy state6.
Shockwave therapy not only moderates inflammation, it also alters the biochemical composition of synovial fluid. By reducing the levels of those destructive enzymes and inflammatory mediators, ESWT allows the joint fluid to regain more of its lubricating, nutritive character. A clinical study in dogs with knee OA showed that after a series of focused ESWT treatments, synovial fluid analysis revealed significantly lower MMP-3 enzyme levels compared to pre-treatment, reflecting a drop in cartilage-degrading activity3. Similar findings include decreases in MMP-13 and aggrecanase (ADAMTS-5) expression in joint tissues post-ESWT3. With fewer catabolic enzymes catabolizing cartilage, there are also fewer breakdown fragments polluting the synovial fluid. While direct evidence is still emerging, research suggests that shockwaves might stimulate synoviocytes to secrete more lubricating factors (like hyaluronic acid) or anti-inflammatory mediators as the synovium returns to a balanced state6. Clinically, veterinarians often observe that joints treated with ESWT have less effusion and improved fluid viscosity. Shockwave therapy shifts the joint fluid back toward a healthier profile – thicker, more viscous, and with less inflammatory signaling.
Finally, ESWT stimulates regenerative processes in the joint. The mechanical stimulus of shockwaves induces release of growth factors and promotes new blood vessel formation, with increased expression of VEGF (vascular endothelial growth factor)7. This results in improved synovial blood supply and nutrient delivery to the joint, providing better support for cartilage repair. In OA rats treated with focused shockwaves, cartilage histology was preserved – the treated rats had more glycosaminoglycan content and type II collagen in their cartilage compared to untreated rats, and their joints also showed lower cartilage degeneration scores5,8. Shockwave therapy creates an intra-articular environment where degeneration is slowed and healing is stimulated.
Reducing inflammation and catabolism while fostering repair makes ESWT a particularly promising tool for managing osteoarthritis in veterinary patients.
Conclusion
Focused extracorporeal shockwave therapy induces cellular and molecular changes in osteoarthritic joints that tilt the balance back toward health. By suppressing pro-inflammatory signals like TNF-α, IL-1β, nitric oxide, and pain mediators such as substance P, ESWT effectively calms the synovium. At the same time, it promotes repair mechanisms, increasing beneficial growth factors, enhancing matrix synthesis, and improving blood flow in the joint. Shockwave therapy not only reduces pain and inflammation in the short term, but also helps to restore joint health over the longer term. The synovial membrane resumes a more normal function, the synovial fluid regains protective qualities, and cartilage is better preserved.
ESWT is a valuable tool for the management of joint osteoarthritis. It addresses both the clinical symptoms and the underlying synovial pathology. Incorporating focused shockwave therapy into a multimodal OA treatment plan can improve comfort, increase mobility, and possibly slow the progression of joint degeneration in animal patients. In the fight against osteoarthritis, shockwave therapy works from the inside of the joint out – helping to provide healthy, pain-free movement in veterinary patients.
References
- Wojdasiewicz, P., Poniatowski, Ł. A., & Szukiewicz, D. (2014). The role of inflammatory and anti-inflammatory cytokines in the pathogenesis of osteoarthritis. Mediators of Inflammation, 2014, 561459.
- Belcher, C., Yaqub, R., Fawthrop, F., Bayliss, M., & Doherty, M. (1997). Synovial fluid chondroitin and keratan sulphate epitopes, glycosaminoglycans, and hyaluronan in arthritic and normal knees. Annals of the Rheumatic Diseases, 56(5), 299–307.
- Liu, S., Chen, Q., Zhang, Q., Tao, K., Li, C., Chang, B., ... & Wang, W. (2023). Electroacupuncture combined with extracorporeal shock wave therapy improves pain symptoms and inflammatory factor levels in knee osteoarthritis patients. Heliyon, 9(10), e207713.
- Maier, M., Averbeck, B., Milz, S., Refior, H. J., & Schmitz, C. (2003). Substance P and prostaglandin E2 release after shock wave application to the rabbit femur. Clinical Orthopaedics and Related Research, 406, 237–245
- Zhao, Z., Ji, H., Jing, R., Liu, C., Wang, M., Zhai, L., ... & Xing, G. (2012). Extracorporeal shock-wave therapy reduces progression of knee osteoarthritis in rabbits by reducing nitric oxide level and chondrocyte apoptosis. Archives of Orthopaedic and Trauma Surgery, 132(11), 1547–1553
- Liu, S., Chen, Q., Zhang, Q., Tao, K., Li, C., Chang, B., ... & Wang, W. (2023). Electroacupuncture combined with extracorporeal shock wave therapy improves pain symptoms and inflammatory factor levels in knee osteoarthritis patients. Heliyon, 9(10), e20771
- Wang, C.-J., Wang, F.-S., Yang, K.-D., Weng, L.-H., Hsu, C.-C., Huang, C.-S., & Yang, L.-C. (2003). Shock wave therapy induces neovascularization at the tendon-bone junction: A study in rabbits. Journal of Orthopaedic Research, 21(6), 984–989.
- Zhao, Z., Wang, Y., Wang, Q., Liang, J., Hu, W., Zhao, S., Li, P., Zhu, H., & Li, Z. (2021). Radial extracorporeal shockwave promotes subchondral bone stem/progenitor cell self-renewal by activating YAP/TAZ and facilitates cartilage repair in vivo. Stem Cell Research & Therapy, 12(1), 19.
ELvation Marketing Team
Combining sales and flexible customer support with many years’ in-depth knowledge of medical equipment we offer customized solutions to create value with long-term investments and medical supplies. ELvation’s strength lies in its ability to combine the apparently contradictory needs of improving the standards of patient care by providing high-quality medical technology and good corporate profitability. We have a special partnership with Richard Wolf GmbH as their long-term authorized Sales & Service Team for piezo shockwave systems.